Robin Williams and Martha Stewart can hardly keep it together in this classic cooking segment
"I feel incredibly honored to have grown up in an era where we had this wonderful man."
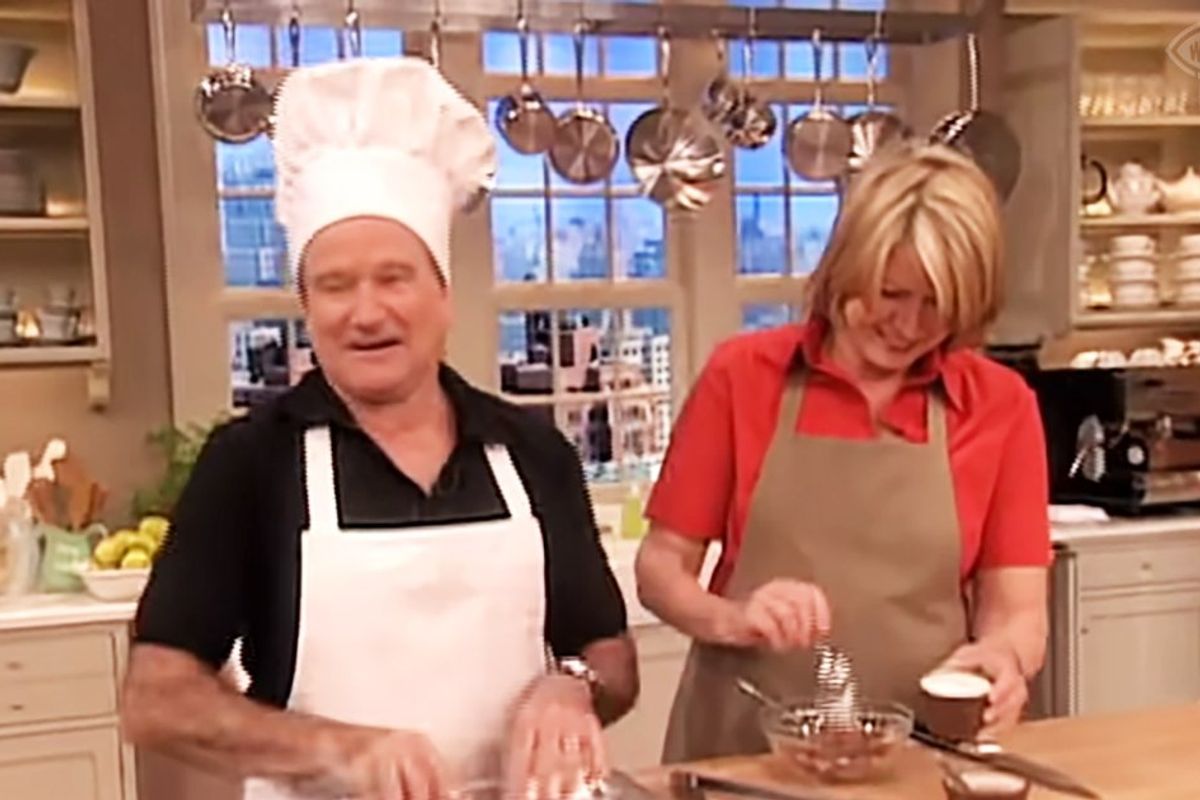
Robin Williams making Martha Stewart crack up.
It's hard to believe it’s been over 10 years since the great Robin Williams left our world. The man left a fantastic legacy of laughs, from his time on TV’s “Mork and Mindy” to his performances in comedy hits such as “Mrs. Doubtfire” and “Aladdin.”
Williams was also an incredible dramatic actor, giving memorable performances in films such as “Dead Poets Society” and “Good Morning Vietnam.”
But the “Comic Relief” star always shined brightest when he improvised on stage, whether on talk shows or in stand-up comedy. One appearance on “Martha Stewart Living” from 2004 has been making the rounds recently because of how quickly he improvised jokes while cooking with Stewart. It’s also great because Stewart plays the perfect straight woman to Williams, although she has a tough time holding it together.
Whenever Stewart mentions an ingredient, whether cumin or brown sugar, Williams turns it into a comedic riff. He also jokes in Spanish and does a few accents that feel off-color 20 years later, but they’re delivered with the best intentions. Williams also walks a bit of a tightrope during the segment while he tries to keep his humor appropriate for daytime TV while reacting to Stewart, who is “rubbing the meat.”
- YouTubeyoutu.be
"I feel incredibly honored to have grown up in an era where we had this wonderful man," the most popular commenter on the YouTube video wrote. "His ability to change characters on the fly is remarkable," another added. "His spontaneous humor is unmatched! He was an incredibly smart, kind and funny man. He is sorely missed!" a commenter said.
Who were Martha Stewart’s favorite guests on her show?
Years later, Stewart would admit that Williams was one of her favorite guests on the show. "We had so much fun because he was the fastest wit and the fastest mind and his mind was like a computer," Stewart told AOL. "No matter what I said, he had a retort and he was so quick. I was marinating meat and he loved that — can you imagine what he did with 'marinating meat' and 'rubbing the meat' and 'ooh la la?' Watch the segment; it's really good."
Martha Stewart relationship advice hits different.
MARTHA, the definitive documentary on the life of the self-made icon, is now playing. pic.twitter.com/wJ55XHZiZU
— Netflix (@netflix) October 30, 2024
What’s the ‘Many Lives of Martha Stewart’ film about?
Although Martha Stewart has rarely been out of the spotlight over the past five decades, she’s been in the news recently after releasing the new Netflix documentary about her life, “The Many Lives of Martha Stewart.”
The film follows Stewart’s journey from teen model to Wall Street stockbroker to the queen of entertaining and good taste. Eventually, she would become America’s first self-made female billionaire. The documentary also discusses the insider trading scandal that sent her to prison in 2004.
The film also reveals Stewart’s guiding philosophy. “I have two mottos. One is: Learn something new every day. And the second one is: When you’re through changing, you’re through,” Stewart says in the film. “Change that garden if you don’t like it. Rip it out and you start all over again.”
If you want to relive the hilarious moments between Stewart and Williams in your kitchen, here’s a recipe for the Chili Espresso Steak Rub.
This article originally appeared last year.
- Billy Crystal's touching eulogy to Robin Williams shows why he was an incredible friend ›
- People are sharing their personal encounters with Robin Williams to honor his birthday ›
- 1991 blooper clip of Robin Williams and Elmo is a wholesome nugget of comedic genius ›
- Harvey Fierstein schooled Barbara Walters on being gay identity in 1983, decades ahead of his time. - Upworthy ›
- Billy Crystal ad-libbed his scenes in 'The Princess Bride' - Upworthy ›
- Martha Stewart is 83, in perfect health, and medication-free - Upworthy ›
- 1984 video of Robin Williams cracking up at his mom's jokes is the perfect comedy origin story - Upworthy ›




 Rihanna Nails GIF
Rihanna Nails GIF
 Good luck trying to catch a gazelle.
Good luck trying to catch a gazelle. Chickens will eat just about anything.
Chickens will eat just about anything. There's actually a big difference between horses and zebras besides just the stripes.
There's actually a big difference between horses and zebras besides just the stripes.