Three moms share how they survived pregnancy related heart failure and symptoms to look for
Black women are at a much higher risk for the rare condition and no one knows why.

Moms share their symptoms of pregnancy related heart failure.
While many view pregnancy as not only natural but a beautiful part of the human experience, it can be easy to forget that pregnancy can also be extremely dangerous. The body goes through many intense changes that can really take a heavy toll: everything from gaining an extra 15 to 30+ pounds and organs being rearranged to make room for a growing fetus, to your heart pumping an excess amount of blood throughout the body.
It can all take an immense toll on the body, which can sometimes lead to serious pregnancy related illnesses like preeclampsia, gestational diabetes, hyperemesis gravidarum, and heart failure. Upworthy spoke with three women during Black Maternal Health Week (April 11-17, 2025) who survived peripartum cardiomyopathy, better known as pregnancy related heart failure. Though the condition is extremely rare, Black women are at a much higher risk of experiencing it though researchers currently aren't sure why.

Tina Marsden, Tracey Young and Tiara Johnson all experienced pregnancy related heart failure during pregnancy or shortly after the birth of their second children. Given their unique experiences, they are all working to make sure other women know what symptoms to look for so they can be treated early to improve chances of survival.
Each of the women had symptoms that could've been brushed off as normal symptoms of pregnancy. In fact, Marsden's symptoms were initially dismissed. "Looking back, I experienced abnormal levels of fluid retention and shortness of breath during my last trimester," she said. "I was already on bedrest due to an incompetent cervix that caused me to start dilating at just 13 weeks into my pregnancy. Even still, my symptoms were considered normal for a high risk pregnancy, instead of being viewed as warning signs for my individual case."

While both Young and Johnson's symptoms were marked by shortness of breath, Young nearly missed the warning sign, telling Upworthy, "Shortly after giving birth to my second child, Amber, I began experiencing shortness of breath. Initially, I attributed this to the physical demands of having just given birth and chose to overlook it. However, as the weeks progressed and the symptoms persisted, I started to wonder if I was developing asthma. I found it difficult to lie flat on my back, and even a brief shower left me feeling exhausted as if I had just run a marathon. After six weeks of these symptoms, I decided to schedule an appointment with my Primary Care Physician."
Johnson also initially dismissed the warning. Having a baby is taxing on the body, so it's unsurprising that some of the symptoms were attributed to recently giving birth. "I was out of breath doing small things like just walking from one room to another. At first, I chalked it up to having just had a baby, but deep down, I knew something wasn’t right. I felt nothing like I did with my first daughter and fatigue was beyond 'new mom tired.' My heart would race, and I felt like I couldn’t breathe both laying down and sitting up."

One might think that recognizing the symptoms would be enough to get the care that is needed, but unfortunately that isn't always the case. Johnson had to visit the hospital multiple times just to get someone to listen to her, she explains to Upworthy: "Yes, I had a lot of trouble. I went to the hospital multiple times before anyone really listened to me. I kept being told it was postpartum anxiety or just stress from being a new mom but it was heart failure. I needed a transplant from the start, but my heart was too weak and my BMI was too high to qualify. I had to fight for every ounce of care I got."
Marsden also found herself fighting to get the medical attention that she initially needed. "While I was under the care of a high risk ob/gyn I still felt like my concerns were not being heard. I encourage expecting mothers to seek a second opinion, and not allow their individual case to be dismissed as 'normal.' There's a thin line between normal symptoms and warning signs of pregnancy induced heart failure, which can have life-altering effects. It's been over two decades since my PPCM diagnosis; and thankfully my Abbott HeartMate II LVAD is helping me to sustain life."

The story of trying to convince medical professionals to take concerns seriously seems to be a common theme, but thankfully Young found a listening ear in her primary care physician. It was during her routine checkup that she mentioned her elevated blood pressure at her last OBGYN check up, Young says the conversation ended there. "After my evaluation, my Primary Care Physician promptly responded to my medical needs by contacting 911, which led to my transportation to the hospital’s emergency room. The hospital cardiologist diagnosed me with Post-Partum Cardiomyopathy. The prognosis I was given was grim, as I was told I would not live to see my daughter turn five."
It was due to the women's determination to advocate for themselves that they're still here to tell their stories to shed light for other expectant moms. The biggest piece of advice all the women give is to listen to your body if something doesn't feel right.

"If you feel unsure about your health or believe something might be wrong, please don’t hesitate to seek medical advice immediately. Having questions is normal, and being your advocate during this time is so important," Young says.
"My advice to expectant moms is not to be afraid or dismissive. Some moms hear stories from others and fear the worst, while others assume those cases are just 'rare' incidents. I encourage expectant moms to consider the experiences shared by advocates like myself as Awareness Tools. Expectant moms should discuss the various Awareness Tools they've come across with their healthcare team to devise a plan that best fits their family's needs," Marsden shares.
"To anyone who feels something is off—please don’t ignore it. Push for answers. Advocate for yourself and don’t stop until you get the care you deserve. You don’t have to be a doctor to know something’s wrong in your body. Never be afraid to get a second opinion," Johnson adds.

Each of these women have become advocates so no other mom has to go through what they have without being armed with knowledge. They were all helped by ABBOTT heart devices that gave their doctors real-time readings of what their hearts were doing. Though, Johnson ultimately ended up getting a heart transplant, she credits her ABBOTT devices with giving her the life she thought she'd lose back to her.
"Receiving a diagnosis of heart failure doesn’t signify the end; instead, it opens the door to a new way of living life. Thanks to numerous medical advancements, people with heart failure can achieve a fulfilling life," reveals Young.




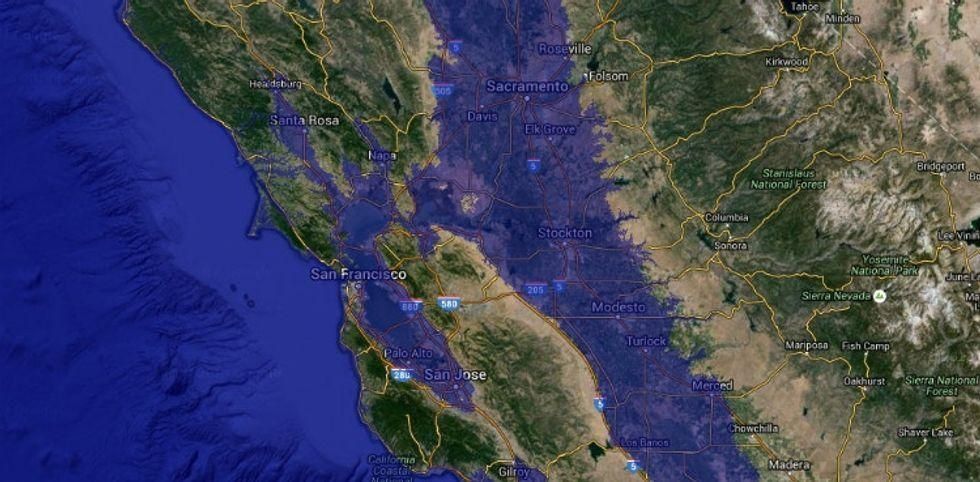
 James Roh
James Roh James Roh
James Roh

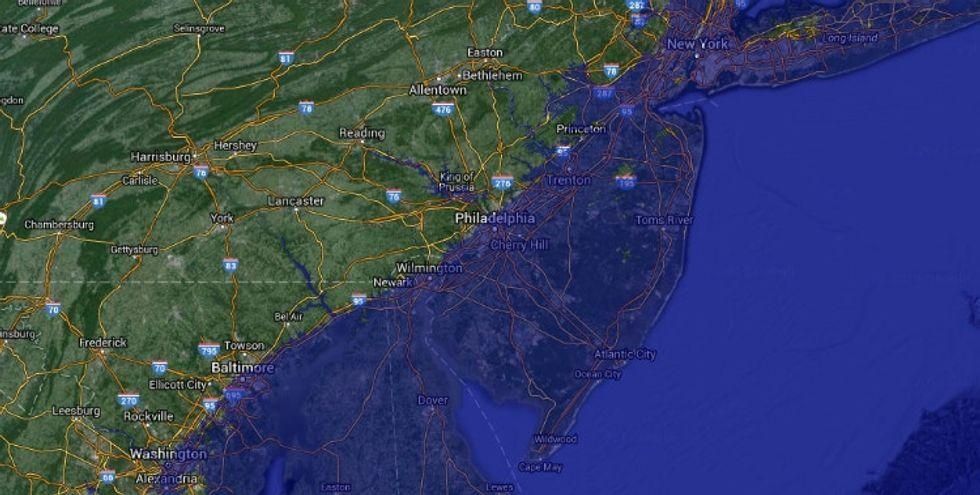
 The Statue of Liberty bears broken shackles at her feet.
The Statue of Liberty bears broken shackles at her feet. The signing of the Declaration of Independence
The signing of the Declaration of Independence The Statue of Liberty symbolizes American freedom and liberty that we're still grappling with.
The Statue of Liberty symbolizes American freedom and liberty that we're still grappling with. The more passionate you are about your goals, the more secretive you should be.
The more passionate you are about your goals, the more secretive you should be.  Senioritis is dangerous for everyone.
Senioritis is dangerous for everyone. If you see something, say something.
If you see something, say something. Young folks enjoying some ice cream outside of a George Orwell mural. via
Young folks enjoying some ice cream outside of a George Orwell mural. via  Sadly, creeps don't need the cover of darkness to be creeps.
Photo by
Sadly, creeps don't need the cover of darkness to be creeps.
Photo by